Just in case you were wondering, I hate rounding with a broiling, incandescent passion.
Unfortunately for me, I’m on my medicine rotation, where rounding is not just a part of the day – it’s THE day. For those of you not indoctrinated into this hateful but necessary practice, rounding is when the “team” – the attending, the resident, the intern, the idiot,* and sometimes other people see all the patients on the list in the morning. You should take the word “morning” with a grain of salt, as sometimes rounds can begin at 6 AM and stretch well into the afternoon. Why this occurs will forever baffle me.
*guess who?!
Before I descend into a rage-driven tirade, I should note that rounding is fundamentally necessary, important, and can be instrumental in patient care. More patient contact is always a good idea, and it absolutely should be the policy of every hospital that every patient gets seen by their primary teams every day – even if it’s only to make sure that some face time occurs. Et cetera.
That said.
I hate rounding. There is no “typical” rounding pattern, because every attending – the physician in charge of the team – has their own style. I’ve been on surgical teams that would review all their patients in a conference room, then split up the list to see the patients in person. This is clearly efficient, if nothing else. Rounds would run a glorious hour maximum. I’ve been on teaching-centered rounds that lasted the entire day, interspersed with short talks and going to see new patients.
I’ve been on “collaborative rounds” on trauma that regularly stretched for seven hours, 6AM to 1PM, because the attending would lecture the team for thirty minutes at each patient’s bedside on a random topic of his choosing – be it ventilator settings, the most recent trial comparing ketamine infusions to propofol drips, or the dreaded potassium homeostasis lecture. I rarely knew what he was talking about, since his lectures were directed toward upper-level residents and fellows, but collaborative rounds mean that nurses, social workers, pharmacists and even family members are around and participate in the rounding process. So it was all the more mystifying that people who had clearly no idea what the guy was talking about would stand there and bear this slow death.
Vulgar yes, hilarious yes, could I resist… no. Bet you didn’t see that coming.
Why do I hate rounding so?
Those of you who know me (hi Grandma, hi Mom) know that I have tremendous, immeasurable patience and an unlimited reservoir of kindness and empathy for the plight of the downtrodden.
Those of you who know me well are now shaking your heads and laughing because I possess none of those things. For short-tempered, impatient people like me, rounding is the horrendous nightmare conference call that never ends.
A typical “round” for me looks like this:
We travel to patient’s door, and I laugh appropriately at a joke made by a superior, which in my case is anyone on the team. I present the patient if it’s “mine;” otherwise, I attempt to look interested while the intern or resident discusses what happened to this person overnight. The most important part of the presentation is the plan, which for the medical student means standing lock-kneed for 20 minutes while the resident and attending discuss minute adjustments to the patient’s diuretic dose and pain medication.
During this torture (“Should we go to forty milligrams? I don’t want to make him too dry. But I want to get more fluid off. But then he will be staying in the hospital another day. But this but that but but but but” MAKE A F%)&#@G DECISION), it is critical to ensure appropriate weight transfer so as to not develop pressure ulcers on my feet from standing still too long.
Finally, after what seems like ages, I watch with gleeful, joyous anticipation as the attending places her hand on the doorknob to the patient’s room and starts to open the door.
Then, disaster strikes. I hear the three most awful words you can hear on rounds:
“Well, what about…?”
NO. THERE IS NO MORE DISCUSSION. We have a plan. We. Have. A. Plan.
But of course… there is more discussion. And now the house of cards we have built has just crumbled into another soul-crushing twenty minutes of standing in the hallway.
 A brief aside and I am not making this up. On one service where we rounded for an average of five hours a day, I would stop on my way in to the hospital and pick up a small, gravel-sized rock from the construction site next to the entrance. Just before rounds would start, I’d deliberately put this rock into my shoe so that when the “Well, what about” question came, and I went into a paroxysmal whole-body muscle spasm out of pure rage, the sharp pain in my foot would serve as a reminder to not turn green, rip off my shirt, and scream “YAAAAAARGGGGHH” Ragemonster Hulk style.
A brief aside and I am not making this up. On one service where we rounded for an average of five hours a day, I would stop on my way in to the hospital and pick up a small, gravel-sized rock from the construction site next to the entrance. Just before rounds would start, I’d deliberately put this rock into my shoe so that when the “Well, what about” question came, and I went into a paroxysmal whole-body muscle spasm out of pure rage, the sharp pain in my foot would serve as a reminder to not turn green, rip off my shirt, and scream “YAAAAAARGGGGHH” Ragemonster Hulk style.
I seriously did the rock thing, every day, for two weeks. It probably prevented me from expulsion, both of my brains and from school.
Anyway. Back to our story. After hearing “Well, what about…” I usually stand there doing deep breathing exercises to prevent a stroke while the team once again debates an esoteric point about whether the patient needs to go to a skilled nursing facility or to a slightly less skilled nursing facility. Eventually, after the next ice age and the extinction of whatever small measure of goodness remains in my being, we finally enter the patient’s room.
This is the payoff, right? Why we “do” medicine. To be with patients, to help them get better, to spend time with them. And during the first two patient encounters of the day, I genuinely feel this way. But by the time we’ve hit the third, we’ve already been rounding for an hour and I can’t deal with it anymore. Once we’ve been in the room for about three minutes, I’m ready to leave and start edging my way toward the door. My body language reads “FLEE!” while the rest of the team, in their infinite patience, stand stoically as the patient and the attending discuss the best way to commute in from the suburbs. Finally – FINALLY – the attending moves toward the door and we move on.
Sometimes.
Yesterday, we sent home a patient who was recently diagnosed with terminal peritoneal carcinomatosis, a horrible abdominal cancer that creates huge quantities of fluid in the abdomen. We had the interventional radiologists place a drain so he could go home and die in relative comfort, and had scheduled an ambulance to pick him up around noon. On rounds we had briefly discussed (HAHAHA there’s no such thing as briefly it took twenty minutes) whether to drain him one last time in the hospital or to have him do it at home later that day, and the attending asked the resident to look into pulling off a last bit of fluid before he left.
On the way back to the room, we ran into the case manager and the patient’s wife discussing timing of the ambulance – whether to go on the ambulance that was coming at 12 or to ask for an hour-long delay and leave at one so we could pull off fluid.
Sound confusing? It wasn’t until we got involved. What ensued was a Dante’s Inferno of absurdity: my resident and the case manager went back and forth for an entire half an hour about the timing of the ambulance. Did it matter in the slightest to the patient? Nope. To use his words, “I don’t give a shit. Just put me on the first ambulance home and stop lollygagging.”
That sounds pretty clear, right? He even used the word lollygagging!
Instead we continued to debate noon versus 1pm. “But if we delay the ambulance for an hour, what if they get called for something else and they don’t come until five? If we start pulling fluid off and the ambulance comes on time, will they wait for us or just go? If if if if if” until the wife finally interrupted. Which was a good thing, because I was about six seconds away from starting my runup for a full-blown swan dive out of the 7th story window, through glass and all.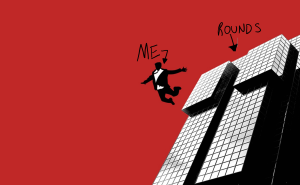
Just to complete the picture, the EMT’s showed up with their stretcher literally as the wife finished her sentence.
Then we went back to rounding. I hate rounds.

I apologize. This is very obviously distributed from my line. Grandma Dorothy was known to say when they gave out patience was in the ladies room
Me too. I couldn’t be a physician, surgeon’s rounds are much quicker!
well i totally get you. on my first day of posting, after standing for about 3 hours, sweating like heck, i felt like fainting and almost vomited right there during a case presentation (round). I just left the group and ran to the toilet and luckily i didnt vomit but i did feel horrible. few minutes later my friend came running and vomited twice!
you describe rounding so distinctly,that i can feel your pain. fortunately, it wont always be like that. you will be in charge. you will know exactly how to torture the med students ,or not. love,grandma
Pingback: Bright Lights, Shiny Objects | Laughter is the Best Medicine
Pingback: The B Pod | Laughter is the Best Medicine
Pingback: Stockholm Syndrome | Laughter is the Best Medicine
Pingback: Helpful Posts | Laughter is the Best Medicine
Pingback: On The Trail | STATUS HAZMATICUS
Pingback: Intern | STATUS HAZMATICUS
Pingback: “Awaiting Return of Bowel Function” | STATUS HAZMATICUS
Pingback: It’s 3 AM And I Wanna Go To Bed | STATUS HAZMATICUS
Pingback: The Liver ICU | crashing resident
Pingback: BUFF and TURF | crashing resident